Cancer has been a formidable foe for medical science for a long time. However, a revolutionary technology known as Chimeric Antigen Receptor T-cell (CAR-T) therapy has recently emerged and is offering a potential solution to combat certain types of cancer. This essay will provide an easy-to-understand overview of CAR-T cell therapy, shedding light on its potential to improve patient outcomes and transform cancer treatment.
How Much Do You Know about CAR-T Cell Therapy?
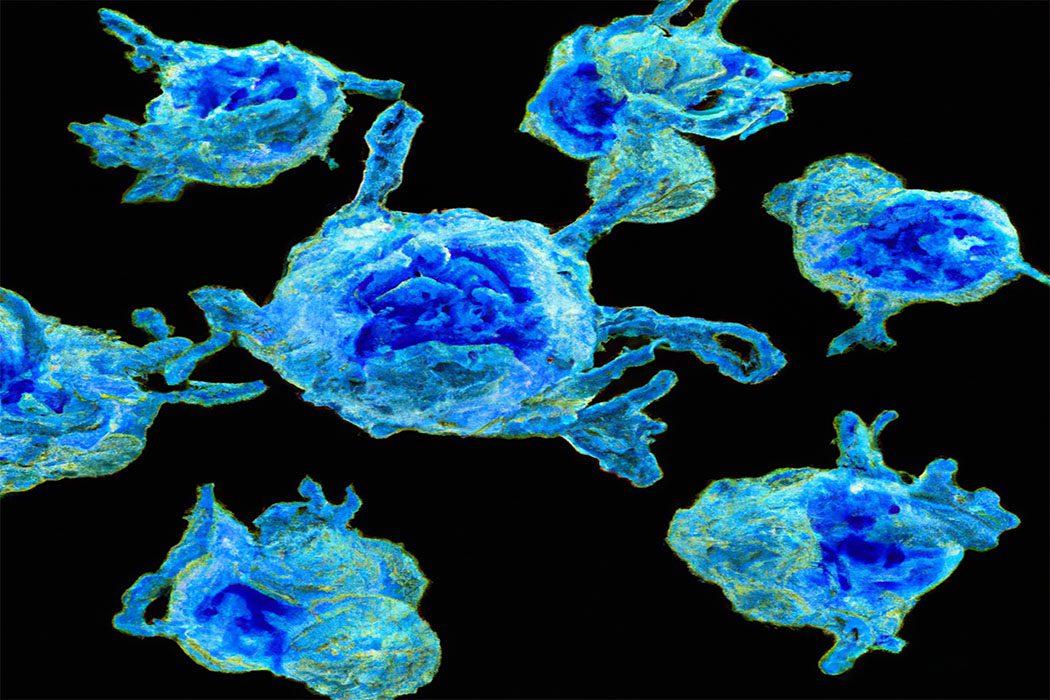
CAR-T Cell Therapy is a type of immunotherapy that is used to treat cancer. It involves the modification of a patient’s own T-cells, which are a type of white blood cells that make up part of the body’s immune system, to recognize and attack cancer cells. CAR-T Cell Therapy is currently the only FDA-approved gene-modified therapy for many types of blood cancers. The story of CAR-T Cell Therapy dates back to 1989 when Zelenetz and his team demonstrated that T cell receptors could be expressed on the surface of certain cancer cells, which formed the basis for chimeric antigen receptors (CARs). This concept was developed over the following two decades, leading to the regimen of CAR-T cell therapy seen today. The core principle underlying CAR-T is to identify a molecule or protein (antigen) on the surface of cancer cells and design a gene-modified T-cell with the ability to recognize and attack those cancer cells. To do this, the CAR-T cell is engineered with a modified virus using a receptor known as a CAR, which is made up of both a cancer-specific targeting antibody and a T cell affinity signaling domain, so as to enable the cell to recognize and target the cancer cells. The resultant CAR-T cells are processed and injected back into the patient’s bloodstream, where they are then distributed around the body and able to identify and attack the cancer cells. Although the process of constructing CAR-T cells is complex, time-consuming, and expensive, it offers a powerful way to target and treat cancer cells and is very effective for some forms of leukemia and lymphoma.
The process of CAR-T Cell Therapy begins by collecting T cells from the patient’s blood and sending them to a laboratory for further genetic modification. T cells have receptors on their surface that allow them to identify and attack cancer cells. The next step is to genetically modify the T cells to express Chimeric Antigen Receptors (CARs) which enable them to more accurately recognize and respond to targets on the cancer cells. This is done through advanced techniques such as gene-editing and transduction. The modified T cells are grown in large quantities and activated to more effectively identify and target the cancer cells. The CAR-T cells are then infused back into the patient’s body, where they can persist for months or even years, allowing the immune system to continuously attack remaining cancer cells and resulting in a long-term immune response that reduces relapse risk. CAR-T Cell Therapy is a revolutionary way to treat cancer that is showing promising results. The process allows for the tailored treatment of individual patients, providing more effective treatment for many types of cancers. In combination with its long-term immune response, it holds the potential to offer a life-changing opportunity to those suffering from cancer.
The CAR, or chimeric antigen receptor, is a protein that combines features of both the T Cell receptor (TCR) and an antibody. It is a fusion protein created by combining an antigen-binding domain from an antibody with either the intracellular signaling domains of a TCR or the cytoplasmic domains of an Fc receptor. The CAR functions as a bridge between the T Cell surface and the antigen-presenting cell, providing T Cells with the necessary recognition site and activating the T Cell’s cytotoxic effector functions. The use of CAR-T cell therapy has dramatically improved the outcomes for previously refractory cancers. The structure of a CAR protein consists of three different domains. The antigen-binding domain enables the CAR to recognize and bind to a specific targeted antigen. This is followed by a hinge domain, which allows the CAR to flex and orient itself in order to maximize its avidity for binding to its target antigen. Finally, a transmembrane anchor domain facilitates linking the CAR to the T cell receptor complex and transmits the signal through the T cell membrane.
The recognition of a specific antigen by CARs is critical for activating the effector functions of the T cell. Specifically, CARs seek out and bind to tumor antigens on the surface of cancer cells, activating the T cell’s cytotoxic functions to attack and kill the cancer cells. This process of antigen recognition is key to the efficacy of CAR-T cell therapy and its success in treating previously refractory cancers. The specificity and selectivity of CARs are determined by a number of factors, including the specificity of the antigen-binding domain, the affinity of the TCR-Fc complex, and the avidity of the Flex hinge domain for the target antigen. The selection of a specific antigen is also an important factor in determining the safety and efficacy of the therapy. Therefore, careful consideration must be given to the target antigen when selecting a CAR for an immunotherapy regimen.
CAR-T therapy has had tremendous success in treating hematological malignancies such as acute lymphocytic leukemia and non-Hodgkin lymphoma in both pediatric and adult patient populations. The success rate of CAR-T therapy for these two blood cancers is estimated to be around 80%, with many patients going into complete remission. The U.S. Food and Drug Administration has approved two CAR-T treatments: Kymriah for treating acute lymphoblastic leukemia and lymphoma, and Yescarta for treating large B-cell lymphoma. While CAR-T therapy has had success in treating hematological malignancies, it is much less successful with solid tumors such as pancreatic, lung, and breast cancer. CAR-T therapy is able to kill some cancer cells, but it is not as effective at targeting the specific mutations present in solid tumors. There are ongoing clinical trials conducting studies to better understand the mechanisms of action and to assess the efficacy of CAR-T therapy and other CAR-T therapies to treat solid tumors. Another challenge with CAR-T therapy is ensuring the safety and efficacy of the treatments, especially with pediatric patients. The side effects of CAR-T therapy can vary, from mild flu-like symptoms to more severe conditions such as cytokine release syndrome and neurological issues. It is critical to monitor patients closely for any potential side effects and to properly manage them. Despite these challenges, CAR-T therapy has had tremendous success in treating hematological malignancies in both pediatric and adult patients, and the currently approved CAR-T treatments, Kymriah and Yescarta, are a testament to that. There is much potential for CAR-T therapy to become effective in treating a variety of solid tumors, and the clinical trials evaluating these therapies are ongoing. CAR-T therapy is an exciting form of immunotherapy that has the potential to offer hope to many cancer patients.
